What Can I Take to Replace Estrogen
Overview
If you're a 40-something woman, you probably have given hormone replacement therapy (HRT) at least a passing thought. As you get closer to menopause age (the average age for menopause is 51.4 years), you'll be giving more serious consideration to questions about HRT. When you reach menopause, will HRT be right for you?
A familiar favorite
As recently as 10 years ago, virtually every woman at menopause automatically got a prescription for estrogen or estrogen combined with progestin, another female hormone. Hormone replacement therapy was standard treatment to relieve hot flashes, vaginal dryness, insomnia and other menopausal symptoms.
Estrogen and the cardiovascular system
Scientists are still learning about the actions of estrogen in the body. Studies have shown that estrogen affects almost every tissue or organ system, including the heart and blood vessels. Estrogen's known effects on the cardiovascular system include a mix of positive and negative:
- Increases HDL cholesterol (the good kind)
- Decreases LDL cholesterol (the bad kind)
- Promotes blood clot formation, and also causes some changes that have the opposite effect
- Relaxes, smooths and dilates blood vessels so blood flow increases
- Soaks up free radicals, naturally occurring particles in the blood that can damage the arteries and other tissues.
Estrogen probably affects the cardiovascular system in other ways that are as yet undiscovered. New research continues to give scientists and physicians more information – and raise more questions about this important and controversial hormone.
Over the years, evidence was accumulating that suggested estrogen also helped protect women against heart disease. With heart disease is the number one killer among women over age 65, this is an important issue. Women develop heart disease 10 years later than men, but by age 65, their risk is equal to that of men.
The accepted thinking was that the drop in estrogen levels associated with menopause accounted for this jump in heart disease risk in women. When estrogen levels decline, levels of LDL cholesterol (the harmful kind) increase, and levels of HDL cholesterol (the positive kind) decrease, leading to the build up of fat and cholesterol in the arteries that contributes to heart attack and stroke. It made sense that replacing estrogen through HRT would potentially improve heart health. This thinking contributed to a huge rise in the number of women being prescribed estrogen.
Rethinking old ideas
Recent studies on the long-term use of HRT are changing that way of thinking. With scientific data potentially linking HRT to higher risks of heart attack, stroke and other serious health problems, many women are reconsidering HRT.
The buzz about estrogen started in the late 1990s when a report from the Heart and Estrogen-Progestin Replacement Study (HERS) was published in the Journal of the American Medical Association (JAMA). This study of more than 2,700 women with existing coronary heart disease was designed to test whether estrogen plus progestin would prevent a second heart attack.
During the first year of HRT, women in the study had a 50 percent increase in heart attack and stroke. But, after two years of treatment, women on HRT actually had less heart disease and fewer heart attacks and strokes compared with women not taking HRT.
The study left many unanswered questions, leading researchers to take another look at these same women. They published their results in 2002. This time around, after nearly three more years of followup, the researchers concluded that there was no lasting decrease in heart disease or heart attack/stroke risk from HRT, and HRT increased the risk of blood clots.
Evidence adding up
Meanwhile, an even larger study, the Women's Health Initiative (WHI), was raising more questions about the potential risks associated with HRT. Involving more than 160,000 women, WHI is the world's largest clinical trial of health interventions for midlife women, studying the effects HRT, diet changes and calcium and vitamin D supplements on heart disease, osteoporotic fractures and breast and colorectal cancer risk.
In 2002, scientists at the National Institutes of Health (NIH) National Heart, Lung and Blood Institute halted the arm of the WHI study in which women were taking combination estrogen and progestin. Early data from this group of women showed that HRT significantly increased the risk of breast cancer, heart attack, stroke and blood clots in the legs and lungs.
Then, in 2004, the NIH stopped the estrogen-only study arm, in which women who had undergone hysterectomy were taking estrogen. Data showed that estrogen increased their risk of blood clots and stroke and did not reduce the risk of heart attack. (Estrogen's effect on breast cancer risk was unclear.)
A change in recommendations
These studies were the first large-scale trials that looked for cause and effect with heart disease and HRT. HRT does offer some benefits, such as preventing osteoporosis and reducing the risk of colon cancer. But the data on heart-related risks from these studies were very compelling. As a result, the American Heart Association and the U.S. Food and Drug Administration developed new guidelines for the use of HRT:
- HRT should not be used for prevention of heart attack or stroke.
- Use of HRT for other problems such as preventing osteoporosis should be carefully considered and the risks weighed against the benefits. Women who have existing coronary artery disease should consider other options.
- HRT may be used short-term to treat menopausal symptoms.
- Long-term use is discouraged because the risk for heart attack, stroke and breast cancer increases the longer HRT is used.
The bottom line, say physicians at the Miller Family Heart, Vascular & Thoracic Institute at Cleveland Clinic: weigh the benefits of HRT against the risks and discuss the whole subject of HRT with your physician to be able to make an informed decision.
Post Menopausal Hormon Replacement Therapy
How prevalent is heart disease among women?
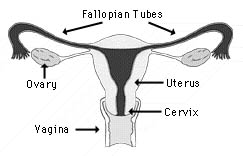
Female Reproductive Organs
Cardiovascular disease is NOT just a man's disease. Cardiovascular disease is the Number 1 killer of women over age 25 in the United States, regardless of race or ethnicity. Once a woman reaches the age of 50 (about the age of natural menopause), the risk for heart disease increases. In young women who have undergone early or surgical menopause, the risk for heart disease is also higher, especially when combined with other risk factors such as:
- Diabetes
- Smoking
- High blood pressure
- Elevated LDL (low density lipoproteins) cholesterol
- Low HDL (high density lipoproteins) cholesterol, sometimes called "good" cholesterol
- Obesity
- Sedentary lifestyle
- Family history of heart disease
What is menopause?
Menopause is a normal stage in a woman's life. The term menopause is commonly used to describe any of the changes a woman experiences either before or after she stops menstruating. As menopause nears, the ovaries gradually produce less estrogen (a female hormone), causing changes in the menstrual cycle and other physical changes. The most common symptoms of menopause are hot flashes, night sweats, emotional changes and changes in the vagina (dryness and atrophy or thinning of the vaginal walls).
Technically, menopause is the end of a woman's reproductive cycle, when the ovaries no longer produce eggs and she has her last menstrual cycle. The diagnosis of menopause is not confirmed until a woman has not had her period for six to twelve consecutive months.
Menopause usually occurs naturally in women between ages 45 and 55 . However, loss of estrogen can also occur if the ovaries are removed during surgery or if a woman goes through early menopause.
How is heart disease associated with menopause?
- Estrogen helps a younger woman's body protect her against heart disease.
- Changes in the walls of the blood vessels, making it more likely for plaque and blood clots to form.
- Changes in the level of lipids (fats) in the blood occur.
- An increase in fibrinogen (a substance in the blood that helps the blood to clot). Increased levels of blood fibrinogen are related to heart disease and stroke.
What can be done to reduce the risk of heart disease for menopausal women?
First and foremost, "traditional" risk factors should be addressed. Women with the lowest risk of heart disease are those who:
- Avoid or quit smoking
- Lose weight and/or maintain their ideal body weight
- Participate in aerobic exercise for 30-40 minutes, three to five times per week
- Follow a diet low in saturated fat (< 7% daily amount); low in trans-fat (partially hydrogenated fats such as margarine or shortening); and high in fiber, whole grains, legumes (such as beans and peas), fruits, vegetables, fish and folate-rich foods
- Treat and control medical conditions such as diabetes, high cholesterol and high blood pressure that are known risk factors for heart disease
For many years, preliminary observational research showed that HRT could possibly reduce the risk of heart disease in women. It appears that the reason why the observational studies showed women on hormone replacement therapy had less heart disease was likely due to the lifestyles of women who take hormone replacement therapy rather than the medical benefits.
More recent studies of women, such as the Heart and Estrogen/progestin Replacement Study (HERS) and the Women's Health Initiative (WHI) concluded overall health risks exceeded the benefits provided by HRT. Women who participated in the WHI showed an increased risk for breast cancer, coronary heart disease (including nonfatal heart attacks), stroke, blood clots and gall bladder disease. Based on the results of these studies, HRT is not indicated for cardiovascular risk reduction. It should be noted that while one arm of the WHI study concluded (estrogen-progestin), other arms (such as estrogen alone) are ongoing. The American Heart Association states, "The loss of natural estrogen as women age may contribute to the higher risk of heart disease after menopause. However, in light of recent results from clinical trials, the American Heart Association does not advise women to take postmenopausal hormone therapy (PHT, formerly called hormone replacement therapy or HRT) to reduce the risk of coronary heart disease or stroke."
There are other risks and benefits that come from HRT. It is important to discuss the risks and benefits of HRT with your own doctor before making a decision.
What exactly is HRT?
Hormone replacement therapy (HRT) is a treatment program in which a woman takes estrogen with or without progestin (a synthetic form of progesterone). To decrease the risk of uterine cancer in women who have a uterus, progestin is usually prescribed with estrogen.
What are the benefits of HRT?
Benefits of hormone replacement therapy for post-menopausal women, include:
- Increased elasticity of the blood vessels, allowing them to dilate (widen) and let the blood flow more freely throughout the body
- Improved short-term symptoms of menopause such as hot flashes and mood swings, as well as vaginal dryness, dry skin, sleeplessness and irritable bladder symptoms
- Decreased risk of osteoporosis and fractures (broken bones)
- Decreased incidence of colon cancer
- Possible decreased incidence of Alzheimer's disease
- Possible improvement of glucose levels
Is HRT safe?
Short-term hormone replacement therapy is safe for most menopausal women who take HRT for symptom control. However, before HRT is prescribed, make sure you review your medical history with your health care provider. Together, you and your health care provider can decide if you have conditions or inherited health risks that would make HRT unsafe for you. HRT is not recommended for women who have:
- History of prior heart attack or stroke and/or increased risk for vascular disease
- Unexplained vaginal bleeding
- Active or past breast cancer
- Fibrocystic breast disease
- Active liver disease
- Endometrial cancer
- Gall bladder disease
- High risk for blood clots or a history of blood clots
What are the risks of HRT?
The health risks of HRT include:
- Increased risk of endometrial cancer (only when estrogen is taken without progestin) For women who have had a hysterectomy (removal of the uterus), this is not a problem
- Increased risk of breast cancer with long-term use
- Increased risk of cardiovascular disease (including heart attack)
- Increase in inflammatory markers (such as C-reactive protein)
- Increased risk of blood clots and stroke, especially during the first year of use in susceptible women
All women taking hormone replacement therapy should have regular gynecological exams (including a PAP smear). The American Cancer Society also recommends that women over age 50 should:
- Perform breast self-examination once a month
- Have a breast physical examination by her health care provider once a year
- Have a mammogram once a year
What are the side effects of HRT?
About 5 to 10 percent of women treated with HRT have side effects which may include breast tenderness, fluid retention and mood swings. In most cases, these side effects are mild and do not require the woman to stop HRT therapy.
If you have bothersome side effects from HRT, talk to your doctor. He or she can often reduce these side effects by changing the type and dosage of estrogen and/or progestin.
If you have a uterus and take progestin, monthly vaginal bleeding is likely to occur. If it will bother you to have your monthly menstrual cycle, discuss this with your health care provider.
Is HRT the same as birth control?
No. Although women who take birth control pills are also taking estrogen and progestin, the effect is not the same. Women who take birth control pills have not been through menopause and need higher levels of hormones to prevent ovulation. HRT is not a high enough strength to stop ovulation.
After menopause, estrogen levels are low and HRT is used at a low dose to restore hormone levels to a more normal level.
How do I decide if HRT is right for me?
Even the best candidates for HRT need to periodically evaluate if HRT is the right treatment for them. You and your health care provider should discuss your medical history and risk factors, as well as how HRT can be tailored to your needs.
Here are some questions you can ask yourself and discuss with your physician:
- Am I experiencing difficult menopause symptoms?
- Do I have any medical conditions or a family history of certain conditions that might make HRT beneficial for me?
- Do I have any medical conditions or a family history of certain conditions that might make HRT riskier for me?
- Have I considered alternatives to HRT?
What Can I Take to Replace Estrogen
Source: https://my.clevelandclinic.org/health/articles/16979-estrogen--hormones
0 Response to "What Can I Take to Replace Estrogen"
Post a Comment